Effective initiation
Appropriate evidence-based interventions achieve a good beginning that leads to an adequate supply of breast milk and better infant health outcomes.

Transition to at-breast feeding
Appropriate evidence-based breastfeeding supportive practices lead to higher breastfeeding rates and better long-term infant health outcomes.

Effective initiation
Appropriate evidence-based interventions achieve a good beginning that leads to an adequate supply of breast milk and better infant health outcomes.

Transition to at-breast feeding
Appropriate evidence-based breastfeeding supportive practices lead to higher breastfeeding rates and better long-term infant health outcomes.









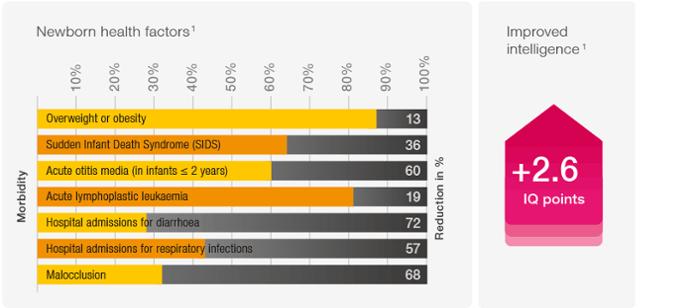
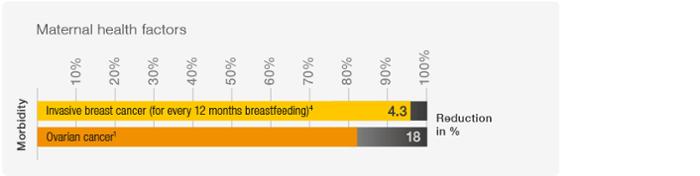 "Every year, breastfeeding could save the lives of 823,000 children below fixe years old, and 20,000 mothers."1
"Every year, breastfeeding could save the lives of 823,000 children below fixe years old, and 20,000 mothers."1