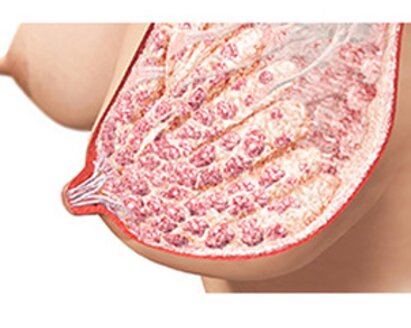
Effective initiation to build and maintain milk supply
Appropriate evidence-based interventions achieve a good beginning that leads to an adequate supply of breast milk and better infant health outcomes.

Transition to at-breast feeding
Appropriate evidence-based breastfeeding supportive practices lead to higher breastfeeding rates and better long-term infant health outcomes.

Effective initiation to build and maintain milk supply
Appropriate evidence-based interventions achieve a good beginning that leads to an adequate supply of breast milk and better infant health outcomes.

Transition to at-breast feeding
Appropriate evidence-based breastfeeding supportive practices lead to higher breastfeeding rates and better long-term infant health outcomes.